| Identification | More | [Name]
Acyclovir | [CAS]
59277-89-3 | [Synonyms]
2-amino-1,9-dihydro-9-((2-hydroxyethoxy)methyl)-6h-purin-6-one
2-AMINO-9-(2-HYDROXY-ETHOXYMETHYL)-1,9-DIHYDRO-PURIN-6-ONE
ACICLOVIR
ACV
ACYCLOGUANOSINE
ACYCLOVIR
ACYCLOVIR SUBST
AKOS NCG1-0055
1,9-dihydro-2-amino-9-((2-hydroxyethoxy)methyl)-6h-purin-6-on
2-amino-1,9-dihydro-9-((2-hydroxyethoxy)-methyl)-6h-purin-6-on
aciclovirum(latin)
aclovir
Acycolguanosine
bw248u
vipral
virorax
w-248-u
wellcome-248u
Acyclovir (Patented-No Supply)
N(9)-Oxyethoxymethylguanine (Acyclovir) | [EINECS(EC#)]
261-685-1 | [Molecular Formula]
C8H11N5O3 | [MDL Number]
MFCD00057880 | [Molecular Weight]
225.2 | [MOL File]
59277-89-3.mol |
| Chemical Properties | Back Directory | [Appearance]
white to light yellow crystal powder | [Melting point ]
256-257°C | [Boiling point ]
366.71°C (rough estimate) | [density ]
1.3654 (rough estimate) | [refractive index ]
1.8000 (estimate) | [storage temp. ]
−20°C | [solubility ]
H2O: 0.7 mg/mL
| [form ]
powder
| [pka]
pKa 2.27 (Uncertain);9.25 (Uncertain) | [color ]
white
| [Stability:]
Stable. Incompatible with strong oxidizing agents. | [Water Solubility ]
Soluble in 1M HCl at 50mg/ml. Soluble in water at 0.7mg/ml. Also soluble in DMSO | [Usage]
Orally active acyclic nucleoside with inhibitory activity towards several herpes viruses. Antiviral | [ε(extinction coefficient)]
11.8 at 256nm at 1mM | [Merck ]
146 | [BCS Class]
4,3 | [InChIKey]
MKUXAQIIEYXACX-UHFFFAOYSA-N | [LogP]
-0.617 (est) | [CAS DataBase Reference]
59277-89-3(CAS DataBase Reference) | [IARC]
3 (Vol. 76) 2000 |
| Safety Data | Back Directory | [Hazard Codes ]
Xi | [Risk Statements ]
R36/37/38:Irritating to eyes, respiratory system and skin . | [Safety Statements ]
S22:Do not breathe dust .
S24/25:Avoid contact with skin and eyes .
S36:Wear suitable protective clothing .
S26:In case of contact with eyes, rinse immediately with plenty of water and seek medical advice . | [WGK Germany ]
2
| [RTECS ]
UP0791400
| [HazardClass ]
IRRITANT | [HS Code ]
29335900 | [Hazardous Substances Data]
59277-89-3(Hazardous Substances Data) | [Toxicity]
LD50 in mice (mg/kg): >10,000 orally; 1000 i.p. (Schaeffer) |
| Hazard Information | Back Directory | [Description]
As it is evident from the chemical structure, acyclovir looks like a nucleoside analog of
guanosine in side chain of which, instead of the traditional cyclic sugar residue a 2-hydrox�yethoxymethyl acyclic side chain is present. Acyclovir possesses antiviral activity with
respect to types 1 and 2 of herpes simplex, shingles virus, Epstein–Barr virus, and
cytomegalovirus. | [Chemical Properties]
white to light yellow crystal powder | [Uses]
Acyclovir (Zovirax) is a synthetic purine analog derived from guanine. It exerts its effects on the herpes simplex virus (HSV) and varicella-zoster virus by interfering with DNA synthesis through phosphorylation by viral thymidine kinase and subsequent inhibition of viral DNA polymerase, thereby inhibiting viral replication. It is effective against HSV-1 and 2, varicella-zoster virus, Epstein-Barr virus, herpesvirus simiae, and cytomegalovirus. Acyclovir may be administered intravenously, orally, or topically.

| [Uses]
Orally active acyclic nucleoside with inhibitory activity towards several herpes viruses. Antiviral; hypnotic. | [Definition]
ChEBI: An oxopurine that is guanine substituted by a (2-hydroxyethoxy)methyl substituent at position 9. | [Indications]
Acyclovir (Zovirax) is a synthetic purine analog derived from guanine. It exerts
its effects on the herpes simplex virus (HSV) and varicella-zoster virus by interfering
with DNA synthesis through phosphorylation by viral thymidine kinase and
subsequent inhibition of viral DNA polymerase, thereby inhibiting viral replication.
It is effective against HSV-1 and 2, varicella-zoster virus, Epstein-Barr
virus, herpesvirus simiae, and cytomegalovirus. Acyclovir may be administered
intravenously, orally, or topically.
Acyclovir (400 mg PO b.i.d. or 200 mg PO five times a day) or other antiviral
antibiotics can suppress herpes-associated EM. It is of no value once the EM has
started. Not all episodes of a herpes simplex recurrence are associated with EM,
but in recurrent cases, a 6-month trial of suppressive therapy can be helpful. | [Manufacturing Process]
Solid sodium nitrite (0.97 g) was added at room temperature with stirring
over a period of one hour to a solution of 2-chloro-9-(2-
hydroxyethoxymethyl)adenine (0.5 g) in glacial acetic acid (10 ml). The
reaction mixture was stirred for an additional 4? hours. The white solid was
removed by filtration, washed with cold acetic acid and then well triturated
with cold water to remove the sodium acetate present. The solid product was
retained. The combined acetic acid filtrate and wash was evaporated at
reduced pressure and 40°C bath temperature and the residual oil triturated
with cold water. The resulting solid material was combined with the previously
isolated solid and the combined solids dried and recrystallized from ethanol to
give 2-chloro-9-(2-hydroxyethoxymethyl)-hypoxanthine (0.25 g), MP>310°C.
Elemental analysis and NMR spectrum were consistent with this structure.
A mixture of 2-chloro-9-(2-hydroxyethoxymethyl)-hypoxanthine (0.375 g) and
methanol (80 ml) saturated with anhydrous ammonia was heated in a bomb
at 125°C for 5 hours. The bomb was cooled in an ice bath and the reaction
mixture removed. Solvent and excess ammonia were removed under reduced
pressure at 50°C. After the residue was triturated with cold water to remove
the ammonium chloride formed, the remaining solid was dried and then
recrystallized from methanol to give pure 9-(2-hydroxyethoxymethyl)
guanine (0.24 g), MP 256.5-257°C. | [Brand name]
Zovirax (GlaxoSmithKline). | [Therapeutic Function]
Antiviral | [Antimicrobial activity]
Activity is restricted to viruses of the herpes group. Herpes simplex
virus (HSV) types 1 and 2, simian herpes virus B and varicella
zoster viruses (VZV) are susceptible to concentrations
readily attainable in human plasma. The 50% inhibitory concentration
(ID50) is 0.1 μmol for HSV-1 and HSV-2 and 3 μmol for
VZV, concentrations much below those toxic to cells. Valaciclovir
is metabolized to aciclovir, and has the same antiviral profile.
Thymidine-kinase-negative HSV mutants and cytomegalovirus
(CMV) do not code for thymidine kinase and are generally
resistant. Although Epstein–Barr virus (EBV) may have reduced
thymidine kinase activity, its DNA polymerase is susceptible
to aciclovir triphosphate and shows intermediate susceptibility.
Human herpes viruses 6 and 7 are less susceptible than EBV. | [Acquired resistance]
Mutations in HSV that involve deficient thymidine kinase
or an altered substrate are most common; alterations in the
DNA polymerase gene also result in resistance. Resistant
mutants may be found in wild virus populations; mutants
lacking thymidine kinase activity may be readily induced
by passage of HSV in the presence of the drug. Resistant
strains have mostly been reported in immunocompromised
patients, are generally thymidine-kinase negative, and have
decreased virulence. Resistant mutants that retain thymidine
kinase activity appear to retain virulence. Emergence of
resistant HSV strains is less frequent in immunocompetent
patients, occurring in about 2% of those receiving prolonged
treatment. | [General Description]
Acyclovir, 9-[2-(hydroxyethoxy)methyl]-9H-guanine (Zovirax),is the most effective of a series of acyclic nucleosidesthat possess antiviral activity. In contrast with true nucleosidesthat have a ribose or a deoxyribose sugar attached to apurine or a pyrimidine base, the group attached to the basein acyclovir is similar to an open chain sugar, albeit lackingin hydroxyl groups. The clinically useful antiviral spectrumof acyclovir is limited to herpesviruses. It is most active (invitro) against HSV type 1, about two times less against HSVtype 2, and 10 times less potent against varicella–zostervirus (VZV).
The ultimate effect of acyclovir is the inhibition of viralDNA synthesis. Transport into the cell and monophosphorylationare accomplished by a thymidine kinase that is encodedby the virus itself.The affinity of acyclovir for the viralthymidine kinase is about 200 times that of the correspondingmammalian enzyme.
use: oral and parenteral. Oral acyclovir is used in the initialtreatment of genital herpes and to control mild recurrentepisodes. It has been approved for short-term treatment ofshingles and chickenpox caused by VZV. Intravenous administrationis indicated for initial and recurrent infectionsin immunocompromised patients and for the prevention andtreatment of severe episodes. The drug is absorbed slowlyand incompletely from the GI tract, and its oral bioavailabilityis only 15% to 30%. Nevertheless, acyclovir is distributedto virtually all body compartments. | [Pharmaceutical Applications]
A synthetic acyclic purine nucleoside analog of the natural
nucleoside 2′ deoxyguanosine, formulated for oral and
topical use, and as the sodium salt for intravenous infusion.
Valaciclovir (the l-valyl ester) is a prodrug formulation supplied
as the hydrochloride for oral use. | [Biological Activity]
Antiviral agent, active against herpes simplex viruses HSV-1 and HSV-2 (EC 50 values are 0.85 and 0.86 μ M respectively). Interferes with viral DNA polymerization through competitive inhibition with guanosine triphosphate. Induces apoptosis in cells transfected with HSV-TK (suicidal gene therapy). | [Biochem/physiol Actions]
Acycloguanosine is an antiviral agent and is converted to acycloguanosine triphosphate by herpes simplex virus thymidine kinase (HSV-TK). It competitively inhibits the viral DNA polymerase. It is less effective against cytomegalovirus and Epstein-Barr virus. Acycloguanosine has been used to study herpes simplex virus latency. It may act against human immunodeficiency virus 1 (HIV-1) as well. | [Mechanism of action]
Acyclovir is a synthetic analogue of deoxyguanosine in which the carbohydrate moiety is acyclic. Because of this difference in structure as compared to other antiviral compounds (idoxuridine, vidarabine, and trifluridine), acyclovir possesses a unique mechanism of antiviral activity. The mode of action of acyclovir consists of three consecutive mechanisms. The first of these mechanisms involves conversion of the drug to active acyclovir monophosphate within cells by viral thymidine kinase. This phosphorylation reaction occurs faster within cells infected by herpesvirus than in normal cells, because acyclovir is a poor substrate for the normal cell thymidine kinase. Acyclovir is further converted to di- and triphosphates by a normal cellular enzyme called guanosine monophosphate kinase. In the second mechanism, viral DNA polymerase is competitively inhibited by acyclovir triphosphate with a lower median inhibition concentration (IC50) than that for cellular DNA polymerase. Acyclovir triphosphate is incorporated into the viral DNA chain during DNA synthesis. Because acyclovir triphosphate lacks the 3′-hydroxyl group of a cyclic sugar, it terminates further elongation of the DNA chain. The third mechanism depends on preferential uptake of acyclovir by herpes-infected cells as compared to uninfected cells, resulting in a higher concentration of acyclovir triphosphate and leading to a high therapeutic index between herpes-infected cells compared to normal cells. Acyclovir is active against certain herpesvirus infections. These viruses induce virus-specific thymidine kinase and DNA polymerase, which are inhibited by acyclovir. Thus, acyclovir significantly reduces DNA synthesis in virus-infected cells without significantly disturbing the active replication of uninfected cells. | [Pharmacokinetics]
Oral absorption, aciclovir: c. 20%
valaciclovir: c. 60%
Cmax 200 mg oral 4-hourly:1.4–4 μmol after 1.5–1.75 h
5 mg/kg 8-hourly intravenous infusion: 43.2 μmol steady state
10 mg/kg 8-hourly intravenous infusion: 88.9 μmol steady state
Plasma half-life: 3–3.3 h
Plasma protein binding: 15%
Absorption
Therapeutic drug levels are readily attained after oral or intravenous administration, although concentrations achieved by an oral dose are over 90% lower than those after intravenous therapy. Accumulation of the drug is unlikely in patients without renal dysfunction. Valaciclovir is readily absorbed and is converted rapidly and almost completely to aciclovir; absorption is unaffected by food. Peak plasma concentrations of 22 μmol are found in subjects after an oral dose of 1000 mg every 8 h; systemic exposure is comparable to that of intravenous aciclovir 5 mg/kg every 8 h. The peak plasma concentration and area under the concentration–time curve (AUC) do not increase proportionally with increasing doses, presumably due to reduced absorption. The time to peak aciclovir concentration is also dose dependent, ranging from 0.9 to 1.8 h after single oral doses of 100–1000 mg.
Distribution
Aciclovir is widely distributed in various tissues and body fluids. Delivery of the drug to the basal epidermis after topical administration is about 30–50% of that obtained by oral dosing. Aciclovir ointment penetrates the corneal epithelium. CSF concentrations are about 50% of simultaneous plasma concentrations. Vesicular fluid concentrations approximate those in plasma. The drug is actively secreted into breast milk at a concentration several times that of plasma. Placental cord blood contains levels of 69–99% of maternal plasma and the drug is 3–6 times more concentrated in amniotic fluid.
Metabolism
About 15% of an intravenous dose is metabolized in persons with normal renal function. The only significant urinary metabolite is 9-carboxymethoxymethylguanine, which has no antiviral activity. Less than 0.2% of the dose is recovered as the 8-hydroxylation product.
Excretion
Around 45–79% of a dose is recovered unchanged in urine, the percentage declining with decreasing creatinine clearance. In patients with renal failure, mean peak plasma concentrations nearly doubled and the elimination half-life increased to 19.5 h. Dosage reductions are advised for various stages of renal impairment. During hemodialysis the half-life is 5.7 h and after dialysis the plasma concentration is about 60% less than the predialysis concentration. Half-lives of 12–17 h have been reported for patients undergoing continuous peritoneal dialysis, with only 13% or less of administered drug being recovered in the 24-h dialysate. The half-life in patients undergoing arteriovenous hemofiltration/dialysis is about 20 h. Less than 1% of a dose of valaciclovir is recovered as unchanged drug in the urine. In multidose studies the amount of aciclovir recovered across dose levels ranged from about 40% to 50%. Between 7% and 12% of the dose is found as the 9-carboxymethoxymethylguanine metabolite. Overall, aciclovir accounts for 80–85% of total urinary recovery. | [Clinical Use]
Aciclovir
Herpes simplex keratitis
Chickenpox and herpes zoster
Herpes simplex encephalitis and neonatal herpes
Prophylaxis of HSV infections in the severely immunocompromised
Valaciclovir
Herpes zoster and genital HSV infections | [Side effects]
Few adverse reactions to topical, ocular, oral or intravenous
formulations have been reported. Allergic contact dermatitis
occasionally occurs with aciclovir cream. Superficial punctate
keratopathy occurs in 10% of patients receiving the ophthalmic
preparation; stinging or burning on application occurs
in 4%. Less common complications include conjunctivitis,
blepharitis and pain.
Transient increases in blood urea nitrogen and creatinine
occur in 10% of patients given bolus injections. It can be largely
avoided by reducing the rate of infusion, adequate hydration
and dosage adjustment in renal failure. Nausea, vomiting,
diarrhea and abdominal pain occasionally occur, particularly
in association with a raised creatinine concentration. Acute
reversible renal failure has been reported. Reconstituted aciclovir
has a pH of about 11; severe inflammation and ulceration
have been reported after extravasation at the infusion
site. Encephalopathy, tremors, confusion, hallucinations, convulsions,
psychiatric disorders, bone marrow depression and
abnormal liver function have occasionally arisen. Skin rashes
have been reported in a few patients but resolve on discontinuation
of the drug.
Headache and nausea have been reported as side effects of
valaciclovir, but occurred with similar frequency in subjects
taking placebo.
Results of mutagenicity tests in vitro and in vivo indicate
that aciclovir is unlikely to pose a genetic risk to humans, and
the drug was not found to be carcinogenic in long-term studies
in mice and rats. No detectable drug-related effects have
been detected in pregnancy. | [Synthesis]
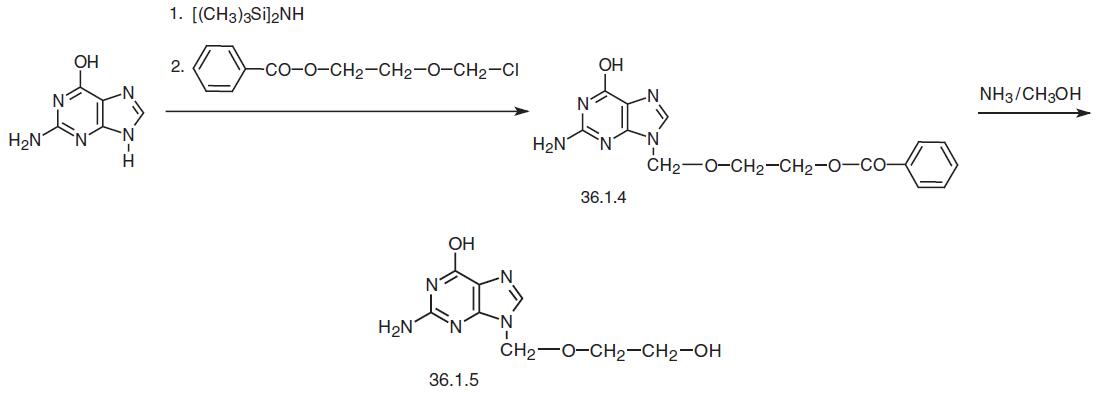
Acyclovir, 2-amino-1,9-dihydro-9-[(2-hydroxyethoxy)methyl]-6H-purin-6-one (36.1.5), is synthesized by alkylating guanine with 1-benzoyloxy-2-chloromethoxyethane in triethylamine. The hydroxyl and amino groups of guanine are previously protected with a trimethylsilyl group by being treated with hexamethyldisilazane. After hydrolysis the result�ing product with water, 9-(2-benzoyloxymethoxymethyl)guanine (36.1.4) is isolated. Treating this with a methanol solution of ammonia removes the benzoyl protecting group from the hydroxyethoxymethyl fragment, giving acyclovir.
Another way of preparing acyclovir begins with 2,6-dichloropurine, which is alkylated with the same 1-benzoyloxy-2-chloromethoxyethane, but in a triethylamine—dimethyl�formamide system to make 2,6-dichloro-9-(2-benzoyloxyethoxymethyl)purine (36.1.6). Treating this with a methanol solution of ammonia replaces both chlorine atoms with amino groups, and subsequent diazotization using sodium nitrite in dilute acetic acid selectively replaces one of the two amino groups for a hydroxyl group, in particular the amino group at position C6 of the purine system. Finally, treating the product with a methanol solution of ammonia removes the benzoyl protection from the synthesized 9-(2-benzoyloxyethoxymethyl)guanine (36.1.4) to make acyclovir.

| [Veterinary Drugs and Treatments]
Acyclovir may be useful in treating herpes infections in a variety of
avian species and in cats with corneal or conjunctival herpes infections.
Its use in veterinary medicine is not well established, however,
and it should be used with caution. Acyclovir has relatively mild activity
against Feline Herpesvirus-1 when compared to some of the
newer antiviral agents (e.g., ganciclovir, cidofovir, or penciclovir).
Acyclovir is being investigated as a treatment for equine herpes
virus type-1 myeloencephalopathy in horses, but clinical efficacy
has not yet been proven and the drug’s poor oral bioavailability is
problematic. There continues to be interest in finding a dosing regimen
that can achieve therapeutic levels and be economically viable,
particularly since the drug’s use during a recent outbreak appeared
to have some efficacy in reducing morbidity and mortality (not statistically
proven). Also, intravenous acyclovir may be economically
feasible to treat some neonatal foals. | [storage]
Store at RT |
|
|